IOL
Latest News
CME Content

In a well-matched sample group, patients with higher levels of postoperative astigmatism reported a greater improvement in quality of life and a greater rate of willingness to have the procedure again if they received an Extended Depth of Focus IOL compared to patients receiving a low-add, multifocal IOL, despite similar postoperative clinical and patient reported performance.

Findings from a pilot study show that a novel accommodative intraocular lens (AIOL, Lumina, Akkolens) provides a true accommodative response that is maintained for at least 2 years and preserved following Nd:YAG laser capsulotomy.

Surgeons work hard to get happy patients, and satisfied patients spread the word and refer their friends. They don't need extra post-op visits, and can return yearly to see their referring doctor. Selecting the best presbyopia-correcting IOL for a patient is critical and depends on methodical, preoperative decision-making.

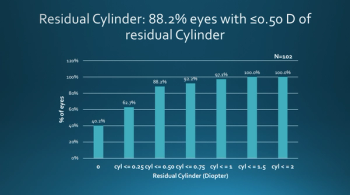
Findings of a study determining the prediction error in the magnitude of residual astigmatism after cataract surgery with a toric intraocular lens (IOL) suggest that use of intraoperative wavefront aberrometry for toric power selection could enhance the refractive outcome in a large subset of eyes.

A prototype of a novel dual-mode, accommodating-disaccommodating intraocular lens with zonular capture haptics has been fabricated successfully. The lens has shown in bench studies to exhibit axial shift and shape change that results in up to about 26 D of accommodative change,

Steven Vold, MD, reports that toric IOLs provide an accurate, safe, and convenient way to correct astigmatism and uncorrected distance vision for glaucoma patients, while patients wanting presbyopic correction have IOL options to fit a range of visual needs.






The WhiteStar Signature Pro (J&J Vision) offers a diverse range of novel technologies that blend together to make cataract surgery easier, safer, and more efficient, according to Steven H. Dewey, MD.

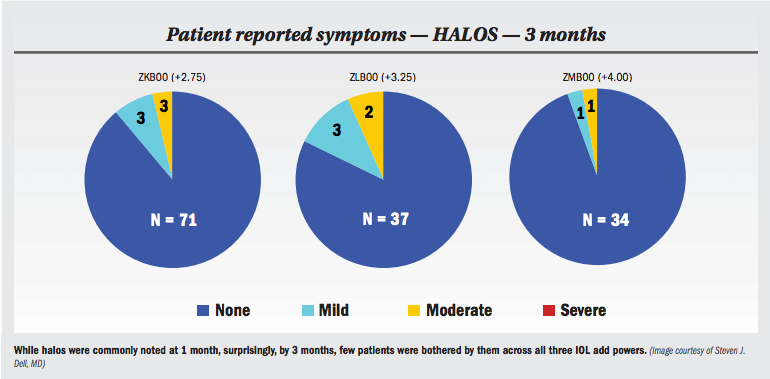
The TECNIS Symfony IOL (J&J Vision) is breakthrough technology that is providing remarkable outcomes and driving a huge increase in the uptake of presbyopia-correcting IOLs among cataract surgery patients, according to Elizabeth Yeu, MD.

Patient selection is the key factor in obtaining the best visual outcomes after cataract surgery and intraocular lens implantation.

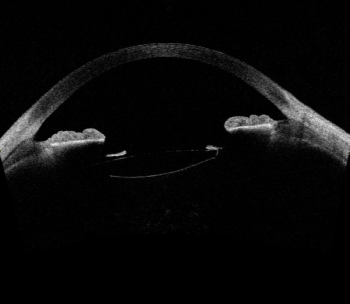
Because a variety of vision-limiting macular pathologies are detectable only with OCT, this imaging should be performed in all patients undergoing cataract surgery.

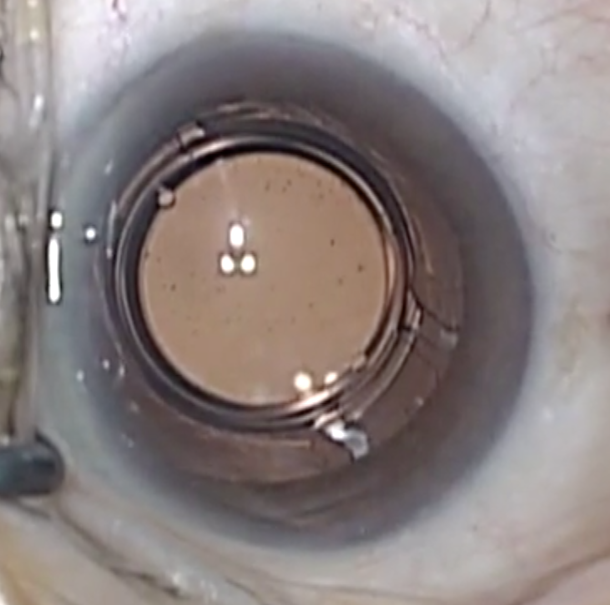
A new small-aperture intraocular lens (IOL) extends patients’ depth of focus as well as multifocal IOLs with fewer dysphotopsias, researchers say.

Scleral tunnel, “glued” fixation technique works better than alternative fixation techniques in cases where intraocular lenses (IOLs) cannot be placed in capsular bag or in the sulcus, according to Sumit Garg, MD.

When it comes to recommending a premium IOL, a patient’s glaucoma is only one factor to consider. Just like any other patient planning cataract surgery, visual needs and preferences for/against glasses are also important factors.

Residual astigmatism is not uncommon after toric IOL implantation. Depending on its cause and magnitude, lens reorientation may be a good solution.

Researchers conducted a 6-month study of patients implanted with the AcrySof IQ PanOptix presbyopia-correcting IOL to determine the binocular defocus curve of the lens. They concluded that these early results show good visual performance across the whole range of defocus. No unexpected adverse events were reported

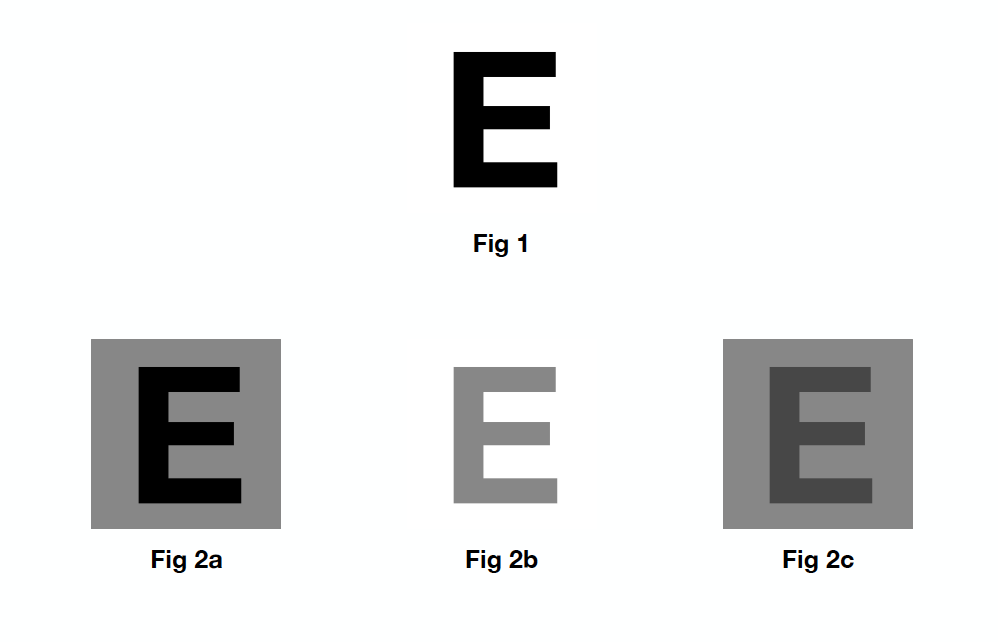
In the past year, Matossian Eye Associates added a new category of presbyopia-correcting IOLs to the practice: the extended depth of focus (EDOF) IOL. The first IOL in this category is the Tecnis Symfony (Johnson & Johnson Vision). EDOF lenses from other manufacturers are in clinical trials, so it behooves the cataract surgeon to better understand how these lenses work.

When dealing with patients with retinal disease, macular disease, or a meaningful risk of retinal detachment, certain types of IOLs should be avoided due to potential complications.