Refractive
Latest News
CME Content













Robert Maloney, MD, shares how a novel system can assist refractive surgeons
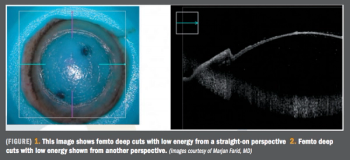
Innovations in procedure may overcome current technical difficulty
Novel agent with mucus-penetrating nanoparticle marries potency, safety, convenience

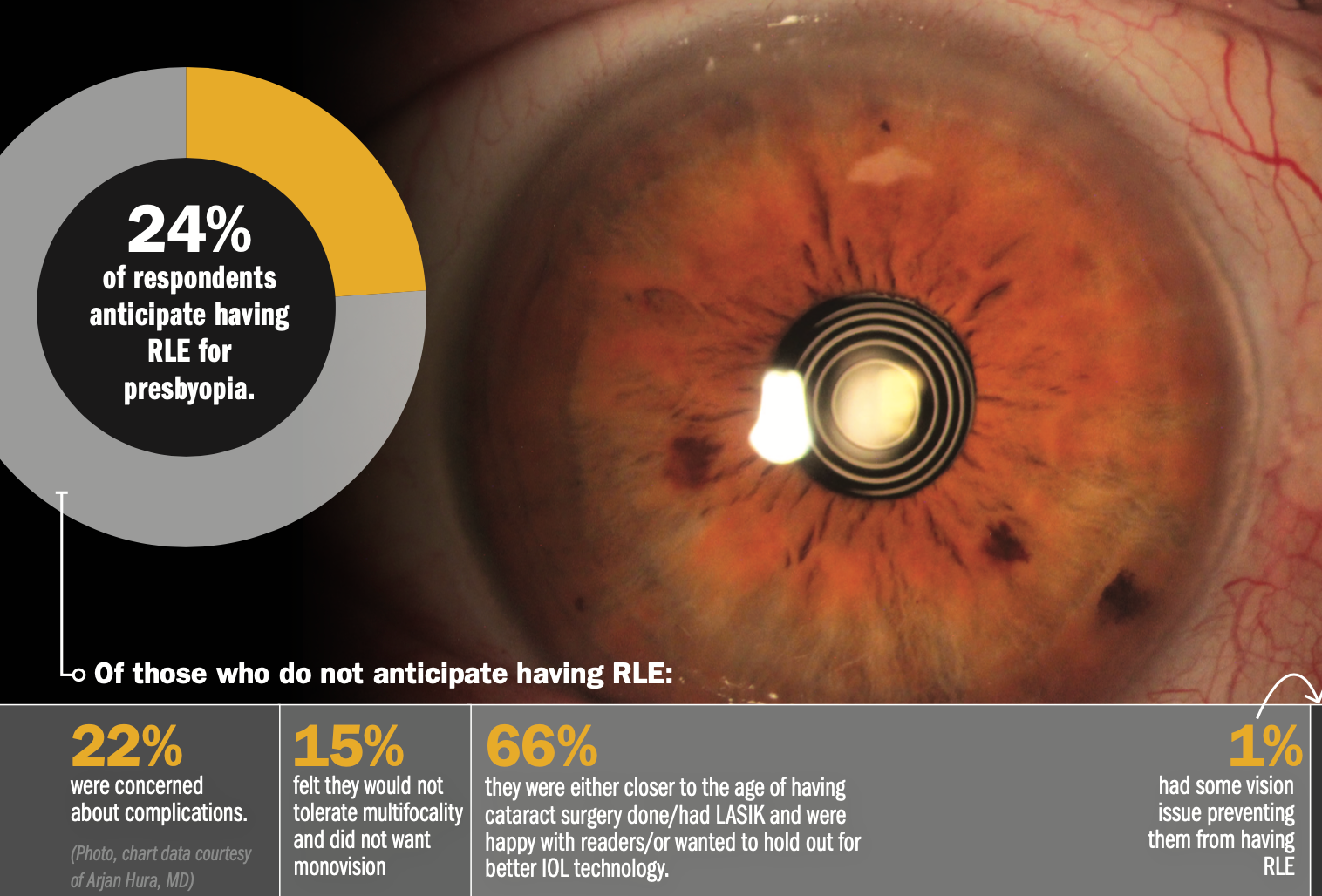
Demographic shifts, improving technology continue to bring patients in at younger age
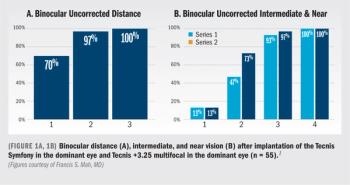
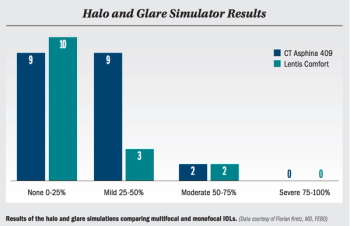
EDOF, multifocal IOLs providing options for patients with range of visual needs

Retina specialist Ron M. Kurtz, MD, details the way collaborative innovation can improve the lives of ophthalmic surgeons, and their patients.

Shan C. Lin, MD, provides the key takeaways from his presentation at the annual Glaucoma 360 meeting.
Adding procedure can improve visual function, offer patients normal lifestyle
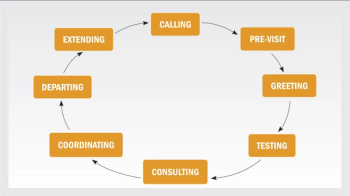
Several points to consider before you make the leap

Improving vision, nonvisual function, quality of life key for customized treatment plans
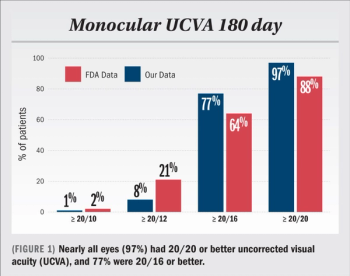
Researchers explore clinical and patient-reported outcomes after WFG LASIK for myopia
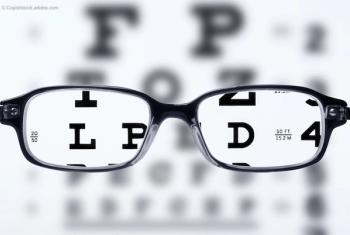
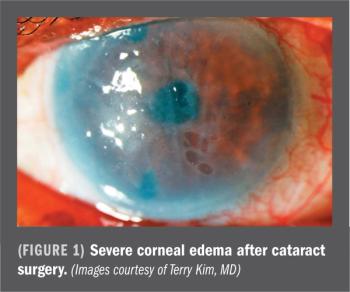
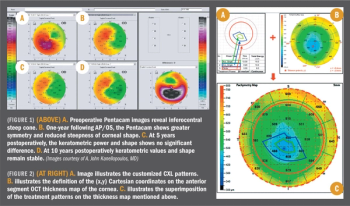
Shortcomings in ablative procedures mean that new developments in refractive surgery are welcome. Arthur Cummings, MD, FRCSEd, reviews two new technologies that will increase patient satisfaction.