Publication
Article
Digital Edition
The role of multimodal imaging in ocular trauma
Closed globe ocular injury often leads to macular pathology
(image Credit: AdobeStock/Lazy_Bear)
The use of optical coherence tomography (OCT) is a cornerstone of retina practice, playing an integral role in the clinical management of most retinal diseases. The technology goes well beyond this use, however, and can also be leveraged in moderate to severe ocular trauma cases.
Whole eye and partial face transplants
In a groundbreaking case published online, a 46-year-old man in Arkansas recently underwent the world’s first whole eye and partial face transplant. Aaron James experienced a traumatic work-related, high-voltage electrical accident that destroyed his left eye and caused him to lose his entire nose and lips, front teeth, left cheek area, and chin, down to the bone.
In May 2023, a large multidisciplinary team from New York University (NYU) Langone Health, in New York, performed the 21-hour transplantation surgery in which the entire left eye and part of the face of a donor were transplanted to James.1 This included the nose, left upper and lower eyelids, left eyebrow, upper and lower lips, and underlying skull, cheek, nasal, and chin bone segments, with all of the tissues below the right eye with the underlying muscles, blood vessels, and nerves; and the left whole eye and socket, including the orbital bones and all surrounding eye tissues and the optic nerve.
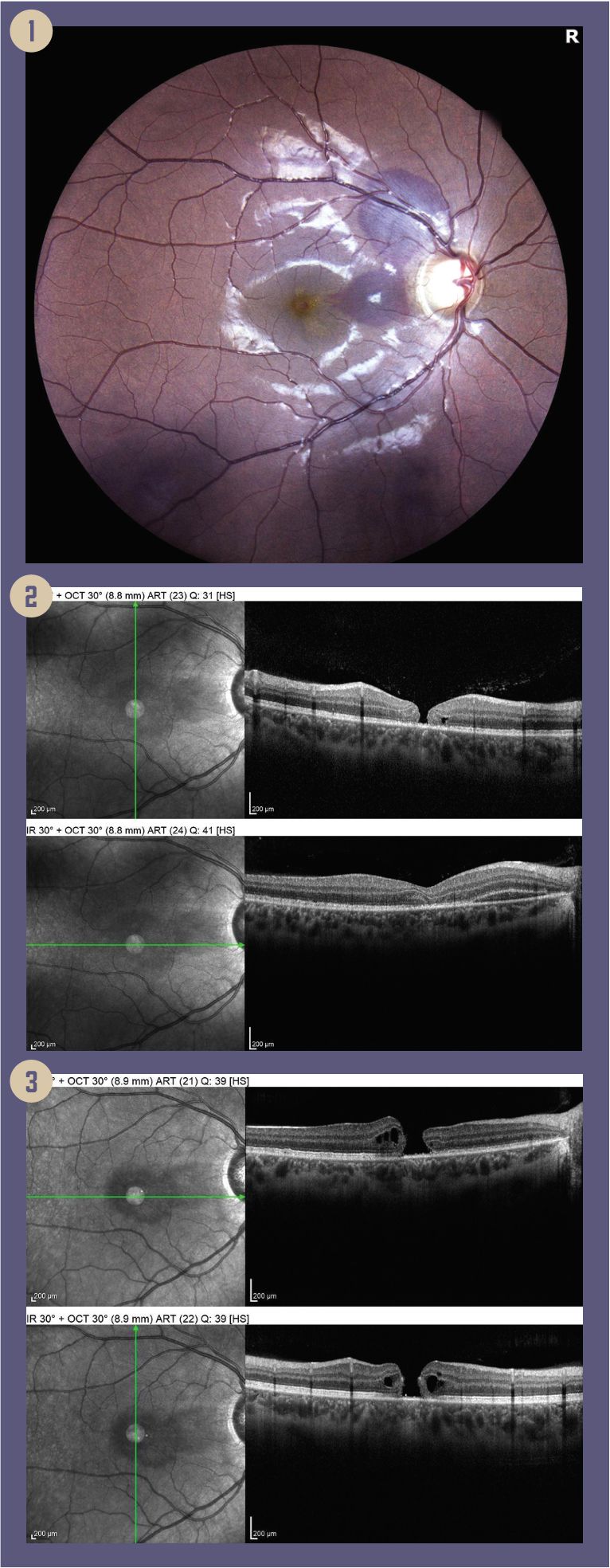
Figures: 1. Traumatic maculopathy, macular hole and subretinal hemorrhage. 2: Macular hole, subretinal hemorrhage, loss of photoreceptor layer. 3: OCT 2 months later, with enlargement of macular hole.
When James experienced severe pain in his left eye after the accident, the Texas surgeons who treated him originally were forced to remove it. The NYU Langone team recommended that the optic nerve be cut as close to the globe as possible to preserve the length of the intraorbital portion of the optic nerve. The team, including one of my peers and lead ophthalmologist and retina specialist Vaidehi S. Dedania, MD, says the transplanted eye is doing remarkably well, in that the retina and globe have a good blood supply and normal intraocular pressure.2 Functional magnetic resonance imaging has indicated that the photoreceptor layer of the retina is responsive to light stimulation. Even though it is not expected that James’ vision will be restored because of optic nerve damage, the results of the surgery are much better than most people expected. Repeated multimodal ocular imaging has been the cornerstone of Dedania’s follow-up on James’ eye.
More than 150,000 corneal transplants are performed worldwide every year. James received the first-ever successful whole-eye transplant made possible by advances in microvascular surgery and the prevention of immune rejection. Restoring vision appears to be the next frontier, limited by central nerve regeneration, specifically the connection between the brain and the optic nerve that must be re-established to restore vision. There are, however, traumatic ocular events that we see more commonly, and we continue to make great strides in technology that enhances our diagnostic capabilities, and helps us preserve and restore sight in these cases.
Open globe injuries
Mechanical trauma to the eye results in either an open globe or a closed globe injury. In an open globe injury, the integrity of the sclera or the cornea has been overcome, resulting in a full thickness wound of the eyewall. This acute situation usually requires immediate surgery to close the wound, which may be caused by a laceration or a rupture. A ruptured globe typically occurs when a significant blunt force is applied to the eye. Lacerating injuries are usually caused by a sharp object, and these injuries are subdivided into penetrating, perforating, and intraocular foreign body (IOFB) trauma.1
The anatomic location of the open globe injury predicts visual potential.2 Zone I trauma involves the cornea and limbus; zone II extends posteriorly from the limbus up to 5 mm posterior to the limbus, involving the lens and zonules; and zone III trauma extends more than 5 mm posterior to the limbus, involving the posterior segment.
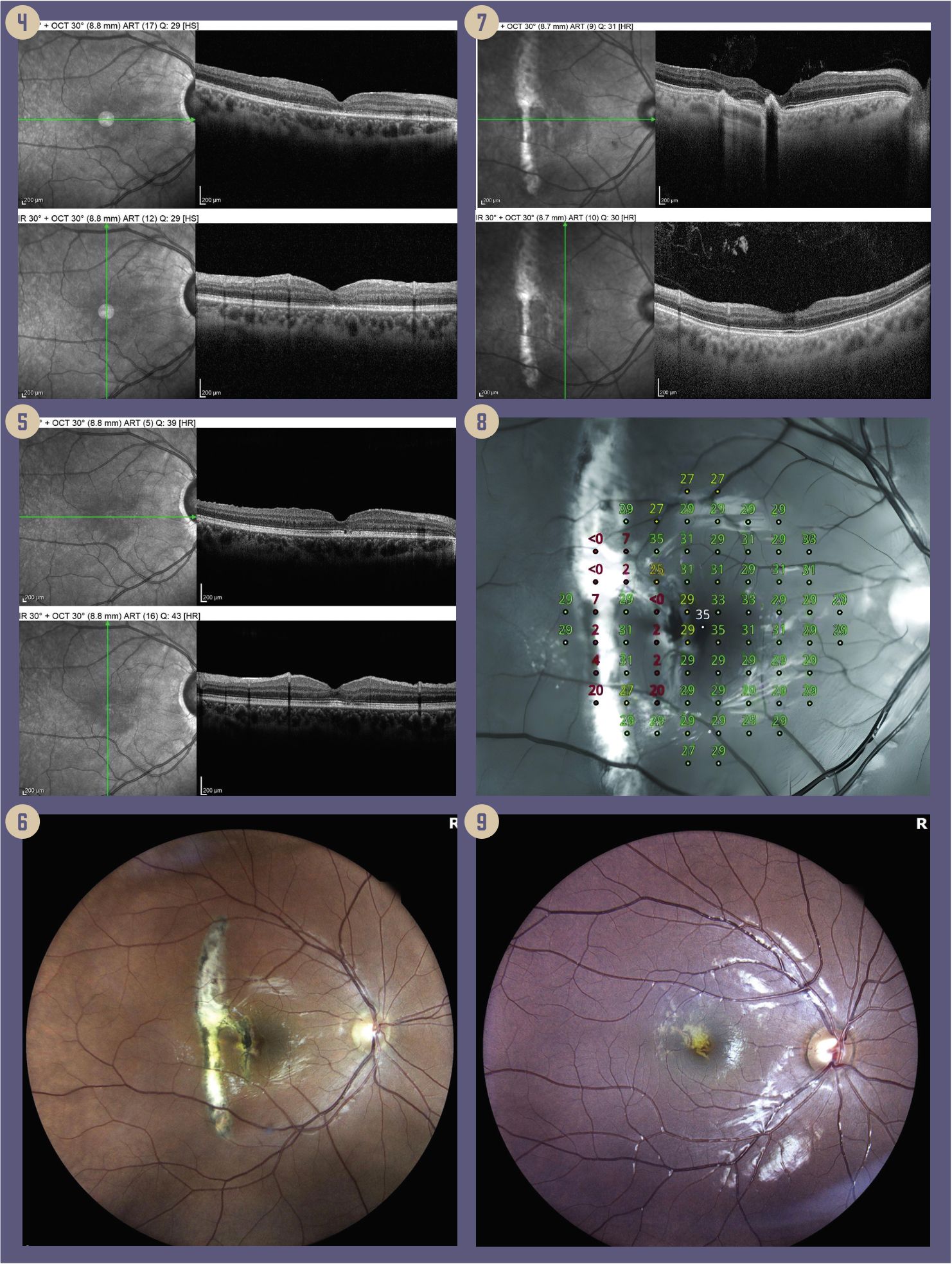
Figures: 4: OCT (post op 2 months) closure of macular hole with resolution of cystoid hydration (Vac 20/50). 5: OCT (post op 1 year) closure of macular hole with resolution of cystoid hydration and improvement in the photoreceptor layer (Vac 20/25). 6: Fundus photo with traumatic choroidal rupture. 7: OCT revealing 2 breaks in Bruch membrane with intact photoreceptors centrally without edema. 8: Microperimetry consistent with paracentral scotoma and preserved 20/20 central vision. 9: A fundus photo with laser
Diagnostic imaging to evaluate the structure of the eye and to rule out the presence of a foreign body is usually done with noncontrast orbital CT. This modality will show globe contour, presence of IOFB, abnormality of the lens, vitreous hemorrhage, retinal detachment, orbital and facial fractures, and obvious orbital volume loss. In some cases, B-scan ultrasonography may be useful in providing information about the posterior segment.
Multimodal imaging’s role in open globe injuries is dependent on the type, severity, and stage of the injury. In the acute phase, only self-sealing full thickness wounds without significant media opacities allow for retina and optic nerve multimodal imaging. Postoperatively, once the media opacities are removed after the primary and secondary repairs, multimodal imaging becomes much more useful in assessing retina or optic nerve edema, proliferation, and signs of inflammation for effective postoperative management. Closed globe injuries, specifically zone III contusion injuries, are most suitable for multimodal imaging.
Closed globe injuries
Closed globe injuries are classified as zone I, the external portion of the globe, including the conjunctiva, sclera, and cornea; zone II, the internal portion of the anterior segment, including the lens, zonules and pars plicata; and zone III, the posterior segment, including the vitreous, retina, optic nerve, choroid, and ciliary body.3
Figures: 10: OCT image of RPE layer. 11: OCT showing decreased flow within the choriocapillaris. 12: OCT after 6 months. (Images courtesy of Ronald Gentile, MD, FACS, FASRS)
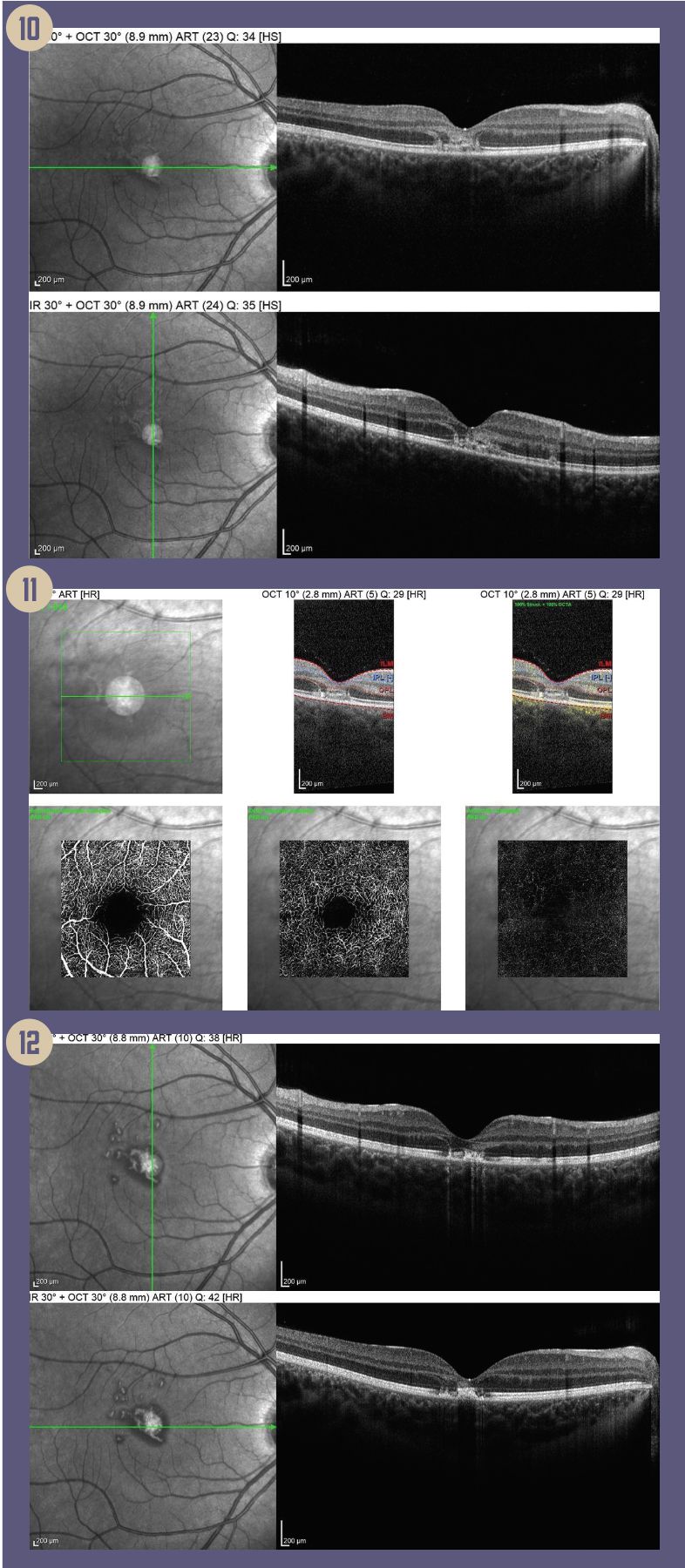
Patients with ocular trauma who are subject to significant blunt force to the globe will more than likely develop some type of posterior segment manifestations that may involve the optic nerve, the vitreous, choroid, retina, or macula. Examples of retinal conditions include Berlin edema (commotio retinae), choroidal ruptures, macular holes, retinal tears, retinal detachment, traumatic proliferative retinopathy, and retinal hemorrhages. Traumatic maculopathy is common, and the cellular-level images like those we can obtain with multimodal OCT become invaluable in these settings. With these detailed images, we can identify macular edema; loss of the photoreceptors; breaks in the internal limiting membrane, external limiting membrane, and Bruch membrane; holes; hemorrhage; cysts; and scars (Case 1, Figures 2-3; Case 2, Figure 7; Case 3, Figures 10-12). In my office, the multimodal Spectralis (Heidelberg Engineering) helps us provide excellent patient care and improve the patient experience by speeding up flow and enhancing efficiency. The platform is excellent when it comes to capturing high quality images through small pupils.
Macular injury can result in a scotoma (Case 2, Figure 8). Other patients can experience a choroidal rupture of the Bruch membrane. Once again, OCT is very helpful in identifying the rupture, and also showing if there is development of a choroidal neovascular membrane. These are conditions that must be treated promptly; a follow-up OCT will confirm successful therapy.
OCT imaging enables visualization and diagnosis of a traumatic macular hole with associated traumatic maculopathy and subretinal hemorrhage after blunt trauma when not readily visible on fundus exam and photo (Case 1, Figures 1-2). High-quality scans are crucial in identifying the full thickness defect in the foveal center with an associated loss of the outer retina, including a moth-eaten ellipsoid zone (EZ) and photoreceptor layer (Case 1, Figures 2-3). Additionally, it aids in measuring subretinal hemorrhage thickness, monitoring its regression, and tracking progression of the macular hole (Case 1, Figures 2-3). In this case, the images confirmed the enlargement of the macular hole with cystoid hydration and retinal pigment epithelial loss 2 months after injury (Case 1, Figure 3). During the postoperative period, imaging allows us to confirm closure of the macular hole with reconstitution of the external limiting membrane and EZ. The most remarkable aspect is the correlation of visual acuity with the reformation of a more robust hyperreflective EZ as observed
on OCT 1 year post-operative (Case 1, Figures 4-5).
Conclusions
In the setting of ocular trauma, OCT is an effective modality for diagnosing and assessing a wide range of posterior segment conditions: Berlin edema, macular holes, submacular hemorrhage, retinal detachment, choroidal rupture and detachment, retinal pigment epithelial tears, optic disc pit, and traumatic retinoschisis. With its high accuracy and precision, the technology is indispensable in my practice for diagnosing and monitoring macular and chorioretinal diseases.
References:
NYU Langone Health performs world’s first whole-eye & partial-face transplant. News release. New York University Langone Health. November 9, 2023. Accessed February 5, 2024. https://nyulangone.org/news/nyu-langone-health-performs-worlds-first-whole-eye-partial-face-transplant
Howard, J. World’s first whole-eye and partial face transplant gives Arkansas man new hope. CNN. November 9, 2023. Accessed February 1, 2024. https://www.cnn.com/2023/11/09/health/first-whole-eye-partial-face-transplant/index.html
Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Graefes Arch Clin Exp Ophthalmol. 1996;234(6):399-403. doi:10.1007/BF00190717
Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, et al. A system for classifying mechanical injuries of the eye (globe). Am J Ophthalmol. 1997;123(6):820-31. doi:10.1016/s0002-9394(14)71132-8

Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.