Ophthalmologists embrace potential of clinically tested nutraceuticals for dry eye disease
Look beyond isolated treatment of the eye to address systemic factors.
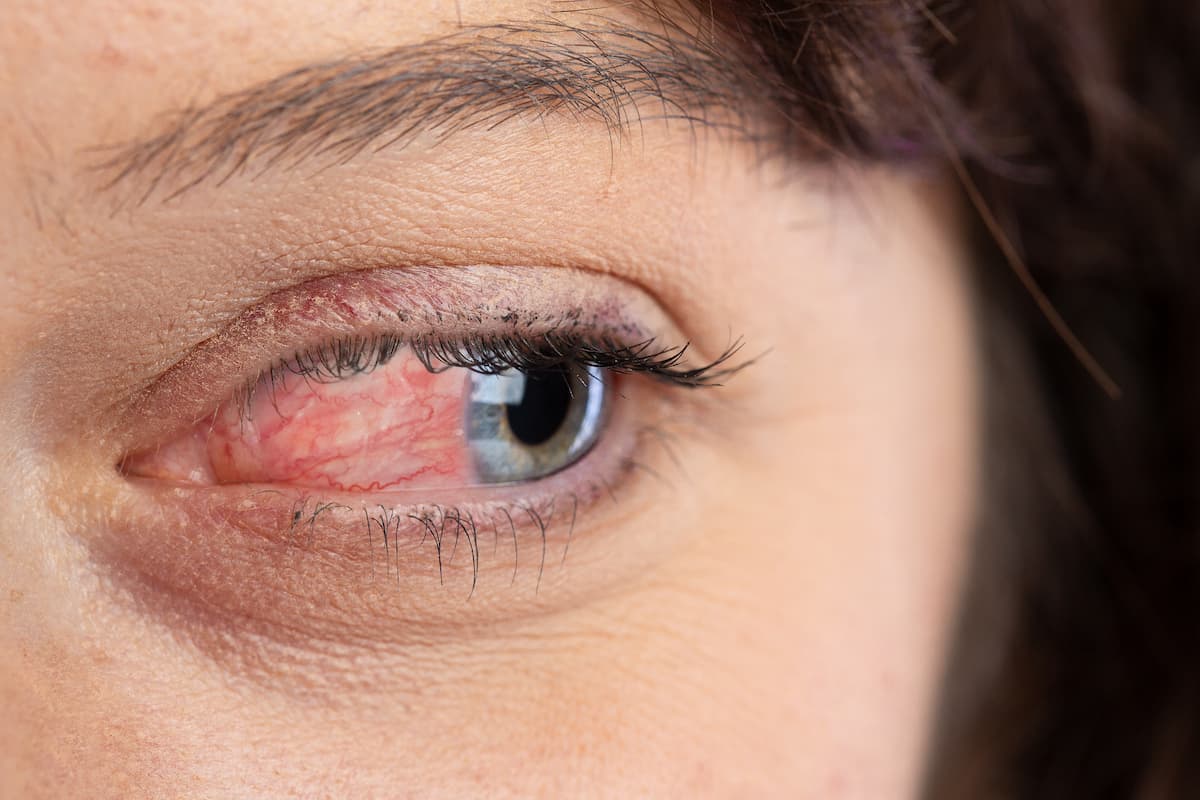
(Image Credit: AdobeStock/Alessandro Grandini)
As medical providers, we look to products and solutions backed by
evidence-based research in order to make the best treatment recommendations for our patients. Many physicians are therefore skeptical of nutraceuticals and oral supplements, which are not often supported by findings from rigorous clinical trials.
In the past, I did not incorporate oral supplementation into treatment regimens due to a general lack of clinical evidence and because I rarely heard supplements discussed from the podium at professional meetings. There are many over-the-counter products, and I knew that ω-3 fatty acid supplements sometimes had disappointing results. When I learned more about the variation in fatty acids and discovered that some have been clinically proven to be effective, however, my approach began to change.
γ-Linolenic acid (GLA) has been shown to help modulate the body’s inflammatory response.1-7 The fatty acid is not found in most ω-3 fatty acid sources such as fish and flaxseed oils, and we do not obtain it from our diets in any meaningful amount.
I was eventually introduced to HydroEye (ScienceBased Health), which contains GLA, and what caught my attention was the fact that the supplement was based in evidence and found to be effective based on findings from a very strong double-blind, randomized, multicenter, controlled trial.8 The trial looked at a multitude of end points, including Ocular Surface Disease Index, impression cytology with immunostaining for inflammatory markers, and topographic corneal smoothness indexes. The high statistical significance found for these markers was remarkable.
In addition to GLA derived from black currant seed oil, the supplement contains eicosapentaenoic acid from highly pure, US Pharmacopoeia–verified fish oil plus other nutrient cofactors that support fatty acid metabolism. The nutraceutical combats inflammation through multiple pathways and is designed specifically for dry eyes.
I began to recommend the supplement to my patients and saw a measurable reduction in symptoms. Dry eye disease (DED) generally requires a multifaceted approach, and I now feel confident including a nutraceutical in my treatment package options. DED is chronic and provides a challenge to patients who are often in populations already dealing with other health issues. Solutions that alleviate part of their load can boost their lifestyle.
Supplementing during preoperative period
I work in a busy surgical practice, and most of my patients come to us for refractive or cataract surgery. Previously, I would recommend other first-line treatments such as lubricating tears and immunomodulatory agents (eg, lifitegrast and cyclosporine) before surgery and wait until post surgery to recommend patients start on a supplement. Although our preferred nutraceutical has been proven effective, it often takes 3 to 5 weeks for patients to experience symptom reduction and 3 to 4 months for them to feel the full effects, and this is generally longer than the window before surgery. Patients have a lot to deal with before their procedure, and I do not want to add more to their load.
I now recommend patients start earlier, prior to surgery. It makes sense to start before surgery so that the supplements are effective earlier in the postoperative phase. We should not assume that patients will not use the supplements due to overload. We can explain that they have DED and that it is a chronic condition with no cure but also that there are many things that can be done to relieve the symptoms, including not only drops but also oral supplementation. I recommend HydroEye to any patient who has ocular surface disease or who will be having surgery likely to trigger ocular dryness.
From my experience, I believe it is important to begin the supplements earlier in the process even if the patient is not symptomatic for DED. Many of our patients have preexisting dry disease, but they’re asymptomatic. After stress to the cornea during surgery, they then develop symptoms.
Other patients may not have DED, but after surgery, they complain of symptoms similar to DED, such as irritation, burning, and fluctuating vision. There is an inflammatory component to this, and dryness is also a culprit. The Refractive Surgery Alliance has coined a new term for the condition: surgical temporary ocular discomfort syndrome (STODS). It is hard to distinguish between DED and STODS, so we treat both with the same tools, and this includes HydroEye.
When evaluating whether a patient would benefit from long-term treatment with nutraceuticals rather than perioperative or short-term treatment, I consider the chronicity of their symptoms and the severity of their dry eye findings on examination. I recommend long-term treatment when I see factors such as heavily inspissated meibomian glands with rapidly diminished tear breakup time, telangiectasias, eyelid erythema, limbal neovascularization, and other signs of chronic inflammation.
Patients with chronic DED are good candidates for nutraceuticals, even in the absence of surgical procedures. In my experience, older female patients generally have disease more refractory to dry eye treatment, and I recommend nutraceuticals to help treat patients with this chronicity.
Reducing the burden
Many of my patients report a reduction in dry eye symptoms when they take the supplements. They tell me that they do not have to use their drops as frequently or that their eyes are not as tired or heavy.
I advise patients to try a supplement for at least 60 days before they decide whether the nutraceutical works for them. I tell patients there is always a chance the supplements might not work for them, but they will most likely find some improvement and may be able to wean themselves off some of their other lubricants. For patients who feel overwhelmed by the number of eye drops they have to use on a daily basis, a nutraceutical can help streamline their dry eye care at home.
I have not seen adverse effects with nutraceuticals, with the exception of one patient who felt a little nauseated. Even this patient said the supplement made her eyes feel better, so she was motivated to continue. I recommend patients take supplements with a meal to avoid stomach discomfort.
In my experience, the rarity of adverse effects and the ease of taking the supplement lead to good adherence. Most of my patients are already taking medication daily, and they just add the supplement to the collection. As long as patients feel improvement, they are motivated to continue.
Conclusion
In our expertise as eye specialists, we sometimes become so focused on the eye itself that we forget the effects of systemic health. We are not always aware of diverse options to attack the root of an ocular problem through multiple pathways and mechanisms. It is important to remember the oral pathway as an option. Not all supplements are the same, and it is valuable to try those that have been clinically proven. Keeping an open mind can lead to an increase in patients’ comfort and a decrease in their drop burden.

Dagny Zhu, MD
E: dagny.zhu@nvisioncenters.com
Zhu is a cornea, cataract, and refractive surgeon; medical director; and partner at NVISION Eye Centers in Rowland Heights, California.
References:
Kapoor R, Huang YS. Gamma linolenic acid: an antiinflammatory omega-6 fatty acid. Curr Pharm Biotechnol. 2006;7(6):531-534. doi:10.2174/138920106779116874
Barabino S, Rolando M, Camicione P, et al. Systemic linoleic and gamma-linolenic acid therapy in dry eye syndrome with an inflammatory component. Cornea. 2003;22(2):97-101. doi:10.1097/00003226-200303000-00002
Macrì A, Giuffrida S, Amico V, Iester M, Traverso CE. Effect of linoleic acid and gamma-linolenic acid on tear production, tear clearance and on the ocular surface after photorefractive keratectomy. Graefes Arch Clin Exp Ophthalmol. 2003;241(7):561-566. doi:10.1007/s00417-003-0685-x
Aragona P, Bucolo C, Spinella R, Giuffrida S, Ferreri G. Systemic omega-6 essential fatty acid treatment and pge1 tear content in Sjögren’s syndrome patients. Invest Ophthalmol Vis Sci. 2005;46(12):4474-4479. doi:10.1167/iovs.04-1394
Kokke KH, Morris JA, Lawrenson JG. Oral omega-6 essential fatty acid treatment in contact lens associated dry eye. Cont Lens Anterior Eye. 2008;31(3):141-146. doi:10.1016/j.clae.2007.12.001
Pinna A, Piccinini P, Carta F. Effect of oral linoleic and gamma-linolenic acid on meibomian gland dysfunction. Cornea. 2007;26(3):260-264. doi:10.1097/ICO.0b013e318033d79b
Brignole-Baudouin F, Baudouin C, Aragona P, et al. A multicentre, double-masked, randomized, controlled trial assessing the effect of oral supplementation of omega-3 and omega-6 fatty acids on a conjunctival inflammatory marker in dry eye patients. Acta Ophthalmol. 2011;89(7):e591-e597. doi:10.1111/j.1755-3768.2011.02196.x
Sheppard JD Jr, Singh R, McClellan AJ, et al. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: a randomized double-blind clinical trial. Cornea. 2013;32(10):1297-1304. doi:10.1097/ICO.0b013e318299549c
