Article
BLOG: Progression of MGD and why early intervention matters
Author(s):
(Image Credit: AdobeStock/liukovmaksym

Meibomian gland dysfunction (MGD) is a progressive disease that begins with mild obstructions (often without any symptoms) and progresses through stages, with worsening gland function, structural changes, and greater impact on the tear film over time. Like other progressive diseases, treatment of MGD is most effective in the earlier stages. Unfortunately, treatment often gets postponed, either because the clinician rationalizes that the condition is “not that bad yet” or because the early-stage, asymptomatic patient doesn’t have a strong incentive to invest in or comply with a treatment regimen.
In my practice, we focus heavily on patient education in the early stages to help patients understand that any gland obstruction is abnormal—and that it will likely get worse if not treated. Objective diagnostic findings (gland imaging, gland function grading, inflammation (MMP-9), and tear osmolarity) are an important part of this education. I show patients how their eyes compare to images of normal, moderate and advanced gland atrophy (Fig 1). The concept of not losing more gland architecture than they already have lost is one that resonates with most patients.
As I discussed in my last blog post, patients with mild to moderate MGD can have obstruction of the glands—meaning they aren’t releasing lipids into the tear film—while having an absolutely normal meibography. I perform standardized diagnostic gland expression using a Korb meibomian gland evaluator to simulate the pressure of the blink on the lids. I count the number of functioning glands and grade the quality of the meibum that is expressed.
Figure 1 . (Image Courtesy Alice Epitropoulos, MD)
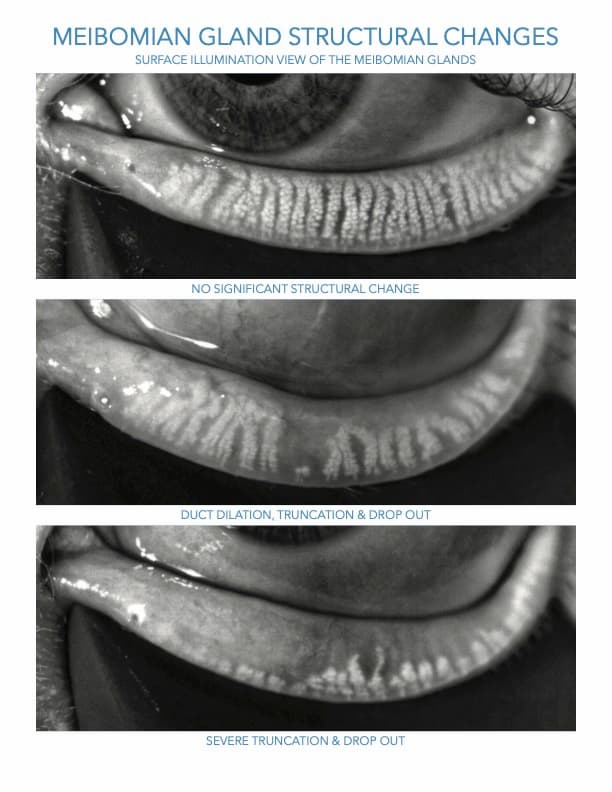
Healthy glands should release meibum with an olive oil-like consistency and appearance. One can expect about one-third to one-half of the lower lid glands to be actively expressing on a given day, with the nasal glands being most active and the temporal glands least active.1 When the gland orifices become capped or plugged, the ducts obstructed, blinking is incomplete, or for those who consume a high ratio of omega 6 to omega 3 fatty acids, trapped oil thickens and becomes more turbid, eventually reaching a toothpaste-like texture (inspissated).1 As MGD progresses, there can be permanent changes to the gland architecture, including atrophy and dropout. Although my colleagues and I have shown that partial recovery of gland structure may be possible,2 earlier intervention to overcome obstruction and poor meibum quality before significant atrophy occurs is ideal.
Vectored thermal pulsation (LipiFlow, Johnson & Johnson Vision) can heat the glands from the inner eyelid surface at a steady 42.5°C temperature while applying pressure to expel obstructions and stagnant material. Although heat and pressure can be applied separately with other technologies, it is more difficult to do effectively and/or may be more challenging to safely direct sufficient heat to the meibomian glands. After thermal pulsation, high-quality re-esterified omega 3 nutritional therapy,3,4 at-home lid hygiene, conscious blinking, and preservative-free lipid-containing tears are more effective and can all help to maintain the newly cleared glands and promote healthy tears.
I explain to patients that healthier tears will spread better and evaporate more slowly so their vision won’t fluctuate as much and they may actually experience less tearing. Poor-quality tears evaporate rapidly, stimulating the production of more (low-quality) tears in an effort to wet the ocular surface, leading to excess tearing. Explaining this counterintuitive symptom to patients is important because many people think they can’t possibly have dry eye if their eyes are frequently tearing.
References:
Tomlinson A, Bron AJ, Korb DR, et al. Th einternational Workshop on Meibomian Gland Dysfunction: Report of the Diagnosis Subcommittee. Invest Ophthalmol Vis Sci 2011;52(4):2006-49.
Hura AS, Epitropoulos AT, Czyz CN, Rosenberg ED. Visible meibomian gland structure increases after vectored thermal pulsation treatment in dry eye disease patients with meibomian gland dysfunction. Clin Ophthalmol 2020;14:4287-96.
Epitropoulos, Alice T, Donnenfeld, Eric D., et al., Effect of Oral Re-esterified Omega-3 Nutritional Supplementation on Dry Eyes. Cornea 2016 Sep: 35(9):1185-1196
Gregory Smith MD, Attending Surgeon Wills Eye Institute Presented at 2011 Cornea Society/EBAA Fall Educational Symposium.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.




