
News















Are older individuals less likely to undergo cataract surgery if they have small support groups? A retrospective cohort study of Medicare patients published in JAMA Ophthalmology looked at this question.

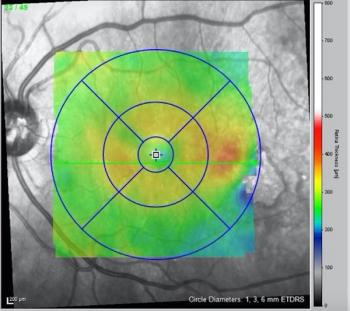
Diabetic eye disease is occurring in younger populations, which means it's time to rethink anti-VEGF standards.

In the first part of his Clinical Innovation series, Josh Mali, MD, shares how this novel home-use device is the new standard of care for AMD monitoring. Future blogs in the series will discuss the increased efficacy of patient monitoring and present case examples.


Stormy Daniels’ pupillary diameter could indicate high intelligence

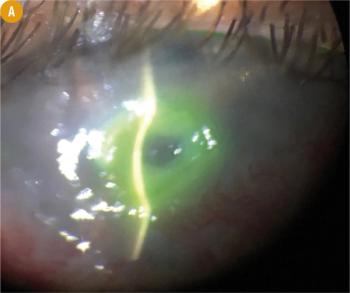
Christopher J. Rapuano, MD, explains how red eye might be something more. Superior limbic keratoconjunctivitis may be identified by lifting the upper lid and having the patient look down.

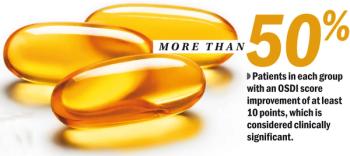
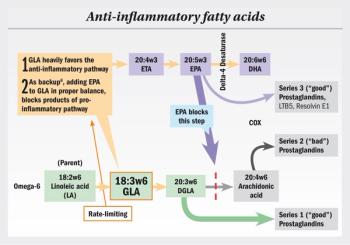
As the diversity of drop products expands and knowledge of the nuances of various ocular surface maladies increases, consider how the differences between drop products might make one drop a better choice for a given patient.

In a well-matched sample group, patients with higher levels of postoperative astigmatism reported a greater improvement in quality of life and a greater rate of willingness to have the procedure again if they received an Extended Depth of Focus IOL compared to patients receiving a low-add, multifocal IOL, despite similar postoperative clinical and patient reported performance.

The title of this blog may have you answering in the affirmative -after all, working in medicine is all about the patients, right?
