Surgical options for painful blebs
A glaucoma specialist discusses surgical treatment options in patients with painful blebs.
Dallas-In patients with painful blebs, surgeons have a few treatment options from which to choose: two filtration revisions and a tube. Ronald Leigh Fellman, MD, talked about how to manage these patients.
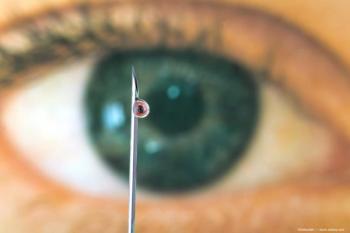
Bleb dysesthesia, defined as a disagreeable sensation produced by ordinary stimuli with decreased vision, pain, and tearing, is present in two-thirds of filtered eyes, more commonly in young patients, blebs located superonasally, and in association with poor lid coverage and bubble formation, according to Dr. Fellman, associate clinical professor emeritus, Department of Ophthalmology, University of Texas Southwestern Medical Center, Dallas.
Limbal-based surgeries compared with fornix-based surgeries seem to have a two-fold greater rate of high and thin avascular blebs, which are more likely to lead to dysesthesia.
“The trend, therefore, is toward fornix-based surgery to avoid bleb dysesthesia,” Dr. Fellman said.
Treatments for bleb dysesthesia include lubrication, bandage contact lenses, bleb needling, compression sutures, YAG laser, autologous blood injection, and cryopexy, which may work in cases in which the problem is limited.
Cases of refractory bleb dysesthesia are more challenging and may require surgery. Three approaches are available. The first two are revisions: autologous conjunctival bleb resurfacing (ACBR) and bleb reduction and conjunctival advancement with Ologen Collagen Matrix Implant (Kestrel Ophthalmics). The third is a bleb excision, with closing of the fistula and insertion of a drainage implant, according to Dr. Fellman.
ACBR is effective but sacrifices valuable conjunctiva from an inferior quadrant that may be needed for an inferior tube, he commented.
Bleb reduction by blunt dissection and conjunctival advancement works well, and Dr. Fellman said he likes to perform this in older patients. The disadvantage is the potential for a bleb leak. This requires undermining of the bleb and conjunctiva to the fornix with care taken to avoid a buttonhole. This is done in order to have tissue that can be pulled forward. In these cases, usually there is flow through the fistula, Dr. Fellman explained.
Ologen, a collagen matrix implant, can be used instead an antimetabolite to inhibit fibrosis and guide the fibroblasts in a favorable way.
“I have had a lot of success in cases of painful refractory blebs,” Dr. Fellman said.
At the end of this surgery, he advised that Tenon’s always be incorporated into the closure using a horizontal mattress closure.
“I like this technique when I want to preserve the bleb,” he said.
In the final surgical approach, which he prefers for younger patients, the bleb is excised and the conjunctiva is undermined so that it can be pulled forward to cover the bleb site. He first uses a pericardial patch graft to cover the fistula, then implants a Baerveldt 350 square hole drainage device in a different quadrant from the bleb location and covers the tube with a corneal patch graft.
Dr. Fellman did not indicate any financial interest in the topic. This article was adapted from Dr. Felllman's presentation during Glaucoma Subspecialty Day at the annual meeting of the American Academy of Ophthalmology.
For more articles in this issue of Ophthalmology Times eReport,
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.