NSAIDs offer potential hope for DR, AMD
Nonsteroidal anti-inflammatory drugs (NSAIDs) are well recognized as potent agents as they block all downstream prostaglandins, have a long history of safety and efficacy, and fare well in extended-release formulations. Recently, there has been a growing body of evidence showing they have potential in treating cystoid macular edema, said Stephen Kim, MD.
Orlando-Nonsteroidal anti-inflammatory drugs (NSAIDs) are well recognized as potent agents as they block all downstream prostaglandins, have a long history of safety and efficacy, and fare well in extended-release formulations. Recently, there has been a growing body of evidence showing that they have potential in treating cystoid macular edema, said Stephen Kim, MD.
This evidence has led to various attempts at developing NSAIDs for the treatment of retinal disorders, said Dr. Kim, Vanderbilt University, Nashville, TN.
The National Eye Institute undertook a study on oral celecoxib to see if it could stabilize or improve vision in patients with age-related macular degeneration (AMD) who are receiving photodynamic therapy (PDT), he said.
Celecoxib is an anti-inflammatory drug that, in animal studies, had prevented the growth of abnormal blood vessels associated with tumors and with injury to the cornea. With that history, celecoxib might reduce swelling and prevent vessel re-growth in AMD, enhancing the effectiveness of PDT, Dr. Kim said. Results were disappointing and the study was halted, he noted.
A separate, more recent study compared oral celecoxib with placebo and diode grid laser with standard Early Treatment Diabetic Retinopathy Study focal laser treatment in 86 participants with diabetic macular edema, but did not find large visual function benefits of treatment with celecoxib or diode laser compared with those of standard laser treatment. A suggestive effect of celecoxib in reducing fluorescein leakage was observed, Dr. Kim said.
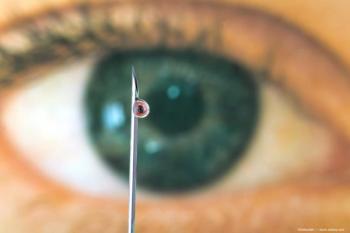
“This illustrates one of the main reasons retinal drugs are delivered intravitreally,” he said.
However, Dr. Kim noted, the drug is 30 times more potent at COX-2 inhibition than ketorolac, but an animal model of intravitreal injection found cataract formation occurred in the 6-mg dose, but not in the 1.5-mg dose.
The Intravitreal Ketorolac for Chronic Inflammation and Retinal Edema Study found favorable shorter-term effects with ketorolac, but the compound was six times more potent at COX-1 inhibition than COX-2.
“(This) rendered it as not a good candidate for intravitreal injection,” he said.
For more articles in this issue of Ophthalmology Times’ Conference Brief, click
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.