Novel use of endoscope helps to visualize hyphema
A glaucoma specialist explores endoscopic visualization for the diagnosis and treatment of uveitic-glaucoma-hyphema syndrome.
Take-home
A glaucoma specialist explores endoscopic visualization for the diagnosis and treatment of uveitic-glaucoma-hyphema syndrome.
Dr. Khaimi
By Mahmoud A. Khaimi, MD, Special to Ophthalmology Times
My primary use for endoscopic visualization has been for the purpose of lowering
The discovery
A colleague referred a male patient who had pseudoexfoliative glaucoma. The patient had undergone prior glaucoma surgery, which controlled his IOP. However, he mysteriously began developing hyphemas, and shortly after, his IOP began to rise.
The patient had a thorough examination of the back of the eye by a retina specialist, and other modalities were used to rule out causes of neovascularization in the retina or elsewhere. After many examinations, my colleagues could not determine why the patient was experiencing recurrent hyphema. The patient was referred to me due to his elevated IOP.
NEXT: Page 2
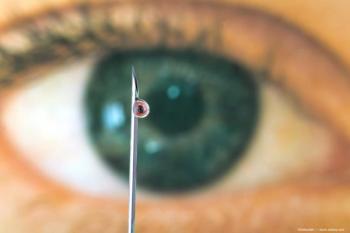
At his initial evaluation consultation, I considered adding a glaucoma drainage implant to lower IOP. I also noted he had pseudophacodensesis and I contemplated whether the patient had a complication with his lens, as he was pseudophakic. The patient underwent surgery on the premise that I would use the ECP laser probe (Endo Optiks) for exploration.
A hyphema washout was performed for clear visibility. The ECP probe was inserted into the anterior chamber through a 1.8-mm clear corneal incision and advanced under the sulcus for visualization of the posterior chamber IOL.
While visualizing the sulcus on the monitor, it was noted that one of the lens haptics had pierced through the capsule and was rubbing against the ciliary processes, causing recurrent hyphema and thus, UGH. The ciliary processes near or adjacent to the haptic that had pierced the capsule displayed atrophy and a white discoloration.
Using one hand to stabilize the ECP probe and the other to hold the MST scissors and forceps (MicroSurgical Technologies), the haptic that was rubbing against the ciliary processes was cut and removed. I was familiar with the anatomy, having performed ECP many times before to lower IOP. I proceeded to perform glaucoma surgery to lower the IOP. Without visualization with ECP, this diagnosis and treatment would have been impossible.
I have since had the opportunity to examine more patients with recurrent hyphema and possible UGH. Despite a negative diagnostic work-up with ultrasound biomicroscopy (UBM) and anterior segment ocular coherence tomography (AS-OCT), all of the referred patients were proven-upon examination with endoscopy-to have a haptic that had either pierced through the capsule or was not placed in the capsule properly.
NEXT: Surgical pearls
Surgical pearls
Though holding the ECP probe in one hand, and the intraocular scissors in the other, can be quite challenging, it can be done. The surgeon must consider the stability of the lens from the start of the procedure and question:
- Whether the lens is stable or unstable (presence of pseudophacodensis or subluxation/dislocation).
- Whether there was a previous complicated surgery that could cause the lens to be more unstable.
- Whether the patient has pseudoexfoliation that can cause more instability to the capsule.
Patients are forewarned that removing the haptic-if it is identified as the source of the recurrent hyphema or uveitis-can lead to instability or dislocation of the lens. Patients may, at a later time, need to have a repositioning of the lens or even a posterior chamber IOL exchange.
NEXT: A notable case referral
A notable case referral
A female patient with idiopathic chronic iritis-which she had been experiencing for 15 years-was referred. She had been seeing a uveitis specialist. One of the mainstay therapies for chronic inflammation is treatment with topical steroids. As expected, after years of being treated with topical steroids, her IOP began to rise. She was then referred to my care.
Upon examination, I noticed a transillumination defect in her iris that appeared to be close to where the haptics might have been. She had an old-fashioned, three-piece IOL implanted 15 years prior. I performed UBM and AS-OCT, which both showed the IOL was in good placement. Upon examination with the ECP probe, half of the patient’s three-piece IOL haptic was in the bag, and the other haptic was rubbing against the ciliary processes. Once again, there was a definitive diagnosis for UGH and a definitive way to treat it, which was to cut away the haptic.
NEXT: Conclusion
Conclusion
All of the patients diagnosed and treated for recurrent hyphema and UGH syndrome have resolved. After following them for 2 years, they have not had any recurrences.
If ophthalmologists look outside the bubble of ECP laser technology and acknowledge access to the smallest endoscope in the world, we can achieve excellent visualization of parts of the eye that we would never be able to see in the office or intraoperatively.
As a result, we have a modality that is minimally invasive and can be used to diagnose and treat recurrent hyphemas definitively. Ophthalmologists who think of leveraging ECP technology this way have the potential 1) to aid in better diagnostic abilities and 2) add another arm to the treatment paradigm.
Mahmoud A. Khaimi, MD, is clinical associate professor, Dean McGee Eye Institute, University of Oklahoma, Oklahoma City. Dr. Khaimi acknowledged no financial interest in the products or companies mentioned. Readers may contact him at
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.