Building the dry eye part of your practice reaps rewards
Dry eye management may be one of the most prevalent, yet overlooked, aspects in ophthalmology.
Key Points
"Dry eye is one of the most common and undertreated diseases in the ophthalmologist's office," said Dr. McCabe, assistant clinical professor of ophthalmology, Vanderbilt University, Nashville, TN. "So many of the patients whom you already are treating for such things as cataract, diabetic retinopathy, glaucoma, and age-related macular degeneration also need to be treated for their dry eye. Once treated, these are some of the most grateful patients in your practice."
Building the practice
"Today, we have a veritable tool box for treating dry eye. We are better able to treat this disease than we were 5 years ago. We have topical cyclosporine (Restasis, Allergan), better-designed punctal plugs with greater comfort and longer retention, and supplemental vitamins (BioTears, Biosyntx; TheraTears, Advanced Vision Research) to help improve patients' quality of tears," he said. "If you help these patients' symptoms so that they now can play outdoor sports, work on their computers, and read more comfortably, they will refer their family and friends."
More women than men seek help for their dry eye symptoms, often complaining of gritty, burning, tearing, red, irritated eyes while doing computer work or reading a novel, Dr. McCabe said. Their vision may blur after reading for more than 10 minutes. "Dry eye is five times more common in females than males," he noted.
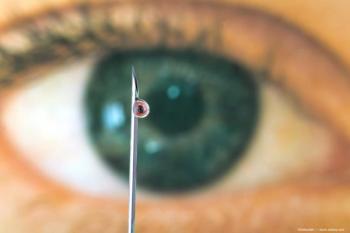
The young female with congested dry-eye symptoms may do well with topical cyclosporine, which works by reducing inflammation by preventing T-cell activation and by allowing the inflamed lacrimal system to secrete higher-quality tears for a healthy ocular surface, he said. In elderly females who are peri or postmenopausal, the quantity of tears is reduced. In this case, Dr. McCabe said he proceeds directly to punctal plugs once artificial tears have failed. "An individual 60 years old only produces 60% of the tear volume that a 20-year-old produces," he said.
Evaluation for dry eye
Dry eye syndrome can be diagnosed using the slit lamp to look for a scant tear meniscus and corneal punctate epithelial erosions, Schirmer test to measure aqueous tear production, and by measuring the tear film break-up time (TFBUT) with fluorescein dye. If the TFBUT is less than 5 to 8 seconds, Dr. McCabe said, then the patient has a significant evaporative component to his or her dry eye. Fluorescein, lissamine green, or rose bengal dye may reveal inferior corneal punctate epithelial erosions.
If the patient has acne rosacea and/or blepharitis, then he or she may have meibomian gland dysfunction, and certain artificial tears containing an oil component can help restore the tear film to its original state, he said. Pseudophakic patients may experience dry eye symptoms after cataract surgery, because povidone-iodine (Betadine) used preoperatively can reduce conjunctival goblet cell density.
Clinicians also should be on the alert for other conditions that can cause dry eye, such as Sjögren's syndrome, sarcoidosis, systemic lupus erythematosus, and rheumatoid arthritis. In each of these cases, the lacrimal gland can be affected, reducing the production of tears. Patients with these conditions are at risk for severe complications of dry eye, such as corneal ulceration and perforation. Topical cyclosporine and punctal plugs can help, Dr. McCabe said. Other causes of dry eye include exposure keratitis from thyroid disease or Bell's palsy and side effects from certain medications such as antihistamines, antidepressants, beta-blockers, diuretics, and oral contraceptives.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.