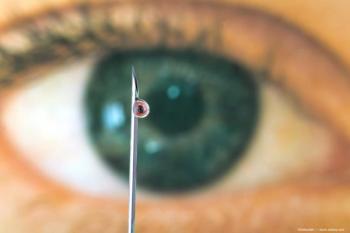
Afferent pupillary defect best predictor of vision survival in rupture, open-globe injuries
The presence of an afferent pupillary defect is the best indicator of visual loss in patients with open-globe injuries, said Michael Grant, MD, PhD, of the Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore.
The presence of an afferent pupillary defect is the best indicator of visual loss in patients with open-globe injuries, said Michael Grant, MD, PhD, of the Wilmer Eye Institute, Johns Hopkins University School of Medicine, Baltimore.
He and his colleagues developed a model by which to predict survival of vision in the presence of rupture and penetrating open-globe injuries. Investigators conducted a retrospective cohort review of 221 patients with open-globe injuries from January 2001 to December 2004. Binary recursive partitioning was used to construct a classification tree to predict vision survival and no vision, he said.
Most patients were men (n = 170) with a mean patient age of 37.6 years. Seventy-three percent of injuries occurred in the home. All patients were treated aggressively and all but one case was closed within 24 hours. The patients were followed for a mean of 8.5 months.
Analysis indicated that an afferent pupillary defect was the most important factor of a possible 14 factors.
"Poor initial visual acuity was an important factor," Dr. Grant said. "The presence of a lid laceration was a contributing factor as well as the presence of a posterior wound."
The constructed model was tested in 51 patients from January to October 2005. The model correctly predicted that vision would survive in 34 patients and was incorrect in three patients. There was no vision survival in 12 patients as the model predicted. The model failed to predict no vision survival in two patients.
"This resulted in 85.7% sensitivity for predicting no light perception and 91.9% specificity for correctly predicting that a patient would achieve no light perception vision or better," Dr. Grant said.
"The presence of a relative afferent pupillary defect appears to be the best prognostic sign of visual loss," he said. "The presence of an eyelid laceration or posterior wound also seems to contribute but was not as statistically powerful. This model seems to do a good job statistically."
He emphasized that a lack of perception vision at presentation is not a reason for patients not to undergo aggressive surgical management for the best possible visual outcome.
Newsletter
Don’t miss out—get Ophthalmology Times updates on the latest clinical advancements and expert interviews, straight to your inbox.